
PDF Download of this Document:
Overview
Per Rectal (PR) and Genital Examinations are taught in the undergraduate medical curriculum and often thought to be an integral part of a complete medical examination.
I am still haunted by bad memories such as being delegated a ‘stand alone’ PR examination on 19 year old girl by a senior resident as an intern. Intimate examination has also been associated with assorted other challenging moments.
None the less, despite being often maligned, some useful information can be gained from these examinations especially in patients with gastrointestinal bleeding, undifferentiated acute abdominal pain or a specific regional complaint. With the PR exam most of the useful information in our experience comes from general inspection and the appearance of the gloved finger. Unfortunately, many of the classically described findings are either subjective (anal tone may be difficult to access) or lacking a good evidence base (PR exam for prostate cancer).
Overall, practical knowledge as well as professionalism and gentleness are important when it comes to intimate examination. The delicate nature of the examination requires clear communication skills, informed consent and the use of a medical ‘chaperone’.
-
These factors come together to make Intimate Emxainations testable in Objective Structure Clinical Examinations (OSCEs).
The PR Examination
The PR examination is commonly performed in patients with a surgical, traumatic and/or neurological complaints presenting to the Emergency Department and Primary Care Clinics.
While it has traditionally been considered essential in many patients it may be overused in some circumstances (particular in low risk trauma cases where it usually adds very little to clinical examination but a lot of stress and anxiety to the patient’s experience of their short hospital stay).
Classic medical teaching has stated that all patients with abdominal pain or trauma should have a PR examination:
Indications and Caveats
There is no clear consensus on the ‘evidence base’ for exactly when to perform PR examinations. However, we can probably discuss where the PR examination should be done (in most circumstances) and where it may be safely withheld.
While I have no special fear or trepidation about doing the PR exam (I have probably done scores of these exams), the bad experiences of several acquaintances after fairly benign road traffic accidents has made me question my practice. Their description of lasting unpleasant visceral memories of a painful gloved finger should make us think twice about doing the PR examination in ‘every patient’ especially where there is a lack of sensitivity or specificity in its utility for making a diagnosis.
When should you do a PR Examination?
A PR exam is necessary in patients with gastrointestinal bleeding to detect fresh blood and meleana. While I would do a PR exam in elderly patients with severe abdominal pain there is emerging evidence that it has a low diagnostic yield and may in fact be harmful. Having said this, a thorough abdominal examination is not considered complete without a PR and/or genital examination. It doesn’t add a huge amount of diagnostic worth in most patients but may be more useful in elderly patients who are at higher risk of malignancy and bleeding.
We suggest considering doing a PR as a part of your assessment in the following circumstances:
PR Examination Considerations:
- Major Clinical Findings to look for:
- meleana, blood on finger, rectal mass, tone, prostate, stool impaction and foreign bodies
PR Examination Demonstration Video
The PR Examination for a ‘Mock OSCE’ (MOSCE)
Communication and Informed Consent are essential components of this ‘MOSCE’ Station:
The PR Examination OSCE Checklist:
- (1) Initial Actions
- Perform Hand Hygiene on entering the Room
- Introduce yourself to the patient
- Check the patients name and wrist band
- Explain the PR examination and obtain consent.
- Explain that a chaperone will be present and reassure the patient of privacy
- Give the patient the opportunity to ask any questions they may have
- Alleviate any anxiety with reassurance and further explanation
- Use a gown if available for infection control
- (2) Prepare Equipment
- Gloves (two pairs of well fitting examination gloves)

- Examination Gel

- Blue Absorbent Pad
- Non Sterile Gown
- Tissue
- Rectal Examination Kit (including Faecal Occult Blood (FOB) Testing)

- (3) Patient Positioning
- Patient should be asked to lie on their left side (left lateral position)
- Use a pillow and cover the patient with sheeting prior and after the examination
- The knees should be drawn up towards their chest
- (4) General Inspection
- Look for redness, injury, skin tags, piles, haemorrhoids, fissures and any discharge
- (5) Internal Examination
- Warn the patient you are commencing examination and use a generous amount of warm lubricant jelly
- Place your finger on the anus so that it points anteriorly
- Apply gentle pressure in the midline and pass the finger into the rectum
- (6) Muscle Tone and Faeces
- Assessment of tone is performed by asking the patient to gently bear down
- Is the felt stool impacted?
- (7) Examine Internally for masses and ulceration by sweeping in two directions. Asking the patient about pain
- (8) In men examine the shape and size of the Prostate – it normally feels smooth and has a groove. In malignancy it may feel craggy and enlarged.
- (9) Remove your finger and look at the glove – place some stool on the wooden spatula and apply a small volume of it to your waiting FOB test kit.
- Remove and dispose of your gloves and gown
- (10) Change gloves and place the FOB reagent on the test and control strips of the FOB
- (11) Thank the patient and wash your hands thoroughly
- (12) Describe your findings to the OSCE Examiner and state examination would be completed by Protoscopy and/or Colonoscopy in this patient
Further Links on PR Examination
- http://www.bmj.com/content/342/bmj.d3421
- http://www.osceskills.com/e-learning/subjects/rectal-examination
- http://bad4umedicine.blogspot.com.au/2012/03/most-rectal-examination-are-pointless.html
The Male Genital Examination
Examination the male external genitalia should be considered in all patients with testicular pain and swelling as well as patients with acute abdominal pain. A head to toe assessment of the diabetic patient with fever may reveal testicular infection and the patient with severe congestive heart failure may also warrant examination. Testicular Torsion in children often presents with abdominal pain as the main complaint so a thorough examnation including genital examination is indicated here.
-
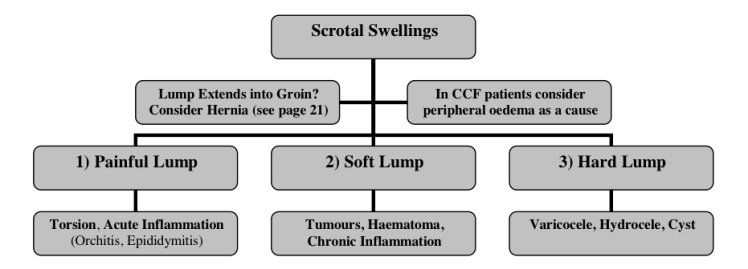
Differential Diagnosis of lumps in the Testes – Hernia, Hydrocele (brightly transluminaties), Tumour (hard localised lump), Torsion (exquisitely tender, emergency), Epididymitis (painful due to inflammation), Varicocele (like a bag of worms, may be due to RCC)
OSCE Exam – External Male Genitalia
Describing a Lump in your OSCE
Checklist for the Examination of a Lump

Testicular Ultrasound Imaging
Ultrasound (USS) has said to be the stethoscope of the 21st century.
USS is especially useful in patients with sudden onset pain to assess for Testicular Torsion (no flow on colour doppler in many cases) and to assess for Epididymo-orchitis (increased flow in many cases)
Ultrasound 1 Epididymo-orchitis – “Testicular US demonstrates increased vascularity in the left testis and epididymis in keeping with epididymoorchitis. There is also a left sided hydrocele.


Ultrasound 2 – Testicular Torsion may be suggested by reduced flow in testes demonstrated on colour doppler studies.

PV Examination
http://www.askdoctorclarke.com
Pelvic examination – for pelvic organs. Use gloves and lubrication. Elevate and steady uterus and adnexae. Determine uterus size (enlarged with pregnancy, fibroids), position (anteverted, axial, retroverted) and mobility of uterus, excitation tenderness (=tenderness that arises in adnexae when broad ligament is stretched by movement of the cervix) and presence of masses.
Cuscoe speculum – to visualise cervix and vaginal walls. For cervical smears and swabs. Dorsal position, insert and rotate to visual cervix (circular in nulliparous, slit in multip).
Sims speculum – to assess uterovaginal prolapse and vesicovaginal fistulae. Use in left lateral position with knees drawn up (L leg straighter supporting other leg). Insert one end into vagina and gently pull backwards to visualise anterior wall. Ask pt to cough to see cystocoele, stress incontinence, cervical descent. To view posterior wall, sponge forceps are inserted to retract anterior wall and speculum is slowly withdrawn. Ask to cough for enterocoele.
Smears – Clearly visualize cervix using bivalve speculum. Insert narrow point of wooden Aylesbury spatula into the endocervical canal. Rotate through 360 degrees in transformation zone (TZ). Spread material evenly on a microscope slide and immerse in fixative. Liquid based cytology is being introduced.
Cervical screening programme – All women between 25 and 50 should have smears taken at 3 yearly intervals, 5 yearly after age of 50 until 65. Screening under 25s is not recommended in guidelines as not cost effective, lots of false positives, very few cancers, high morbidity of loops as likely to want children in future and may need further loops, avoid over treatment as most cases will resolve. Don’t screen over 65s unless never screened before as unlikely to develop new lesions. Screening at 3 yearly intervals picks up 91% of pre-malignant cases, screening yearly would only increase this to 93%. Smears can show mild, moderate or severe dyskaryosis (cytological diagnoses). If mild repeat, if moderate or severe refer to colposcopy. Technically unsuitable smears – about 8% (should be 1% with liquid cytology), due to blood, pus, inflammation, not cells from SCJ or not enough cells.
Swabs – High vaginal swabs are taken from the posterior fornix using a bivalve speculum. These are used to detect lower genital tract pathogens e.g. candida or TV. Endocervical swabs are used to detect pathogens that infect columnar epithelium and may cause PID e.g. Chlamydia and gonorrhoea.





One thought on “Intimate Examinations”
Comments are closed.