Case 3 – Mechanical Ventilation
I recently encountered a challenging clinical case (consented to share here). In the case a patient required a one hour transfer between two hospitals. The young patient had an recessive inherited chronic lung disease and was immunosuppressed They had presented to their local hospital after developing progressive severe shortness of breath over a 24 hour period. This ultimately resulted in the requirement of Rapid Sequence Intubation (RSI) and Mechanical Ventilation. In the Intensive Care Unit (ICU) at the small district hospital the patient was found to be difficult to ventilate on their Puritan Bennett ventilator (pictured).
The Puritan Bennett
ICU Ventilator
Even this high level ICU ventilator was only adequate to maintain a CO2 of around 80 mmHg (with a similar corresponding End Tidal Co2 measurement). In this case there was a significant acute respiratory acidosis and the respiratory rate was set to 30/min in the referring ICU.
On transfer to a portable ventilator, the Oxylog 3000, the CO2 started to gradually rise and the acidosis worsened… Although I was familiar with the device from working in Emergency Departments in the past there appeared to be a significant difference the the set volumes and the received volumes in this (<30kg) Adult patient.
The Oxylog 3000
Emergency Transport Ventilator
The repeat ABGs lead to a CO2 of >100 and worsening acidosis with a conservative lung protective strategy:
Blood Gas 1
With sedation, paralysis and increased minute volume (from respiratory rate) as well as changing the I/E ratio there was some improvement in the blood gas. After planning ongoing transport from the small peripheral hospital to the large tertiary hospital the patient remained stable throughout this process.
While the Oxylog 3000 ventilator continually alarmed due to high peak pressures the measured plateau pressure remained around the 30cmH20 mark. At this point a case conference was initiated and we decided that it was safe to transport the patient with these pressures. In addition, with the appropriate changes described above the ventilation appeared better from the end of the bed and the blood gas improved (with a Co2 around the 90 mark and pH of around 7.1).
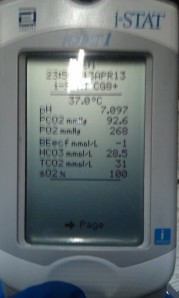
A further blood gas was taken on route (in the helicopter) using an I-STAT machine:
Blood Gas 2
The patient improved over the next 24 hours and it was suspected (with hindsight) that she might have Bronchiolitis Obliterans Syndrome Complicating her Lung Transplant.
Discussion
This case and similar presentations in the past have left me wondering the best ways to ventilate difficult patients in the ED and Pre-hospital environment without high-level ventilators and the immediate expertise of ICU physicians. At the outset I would suggest that early consultation in these cases is extremely useful as is a process of continuous reassessment of the patient from the end of the bed.
In this case it was interesting to note a degree of discrepancy between the settings of the machined and what the patient received. The initial measured lung protective strategy (6-8ml/kg) with a rate of 20/min was inadequate in terms of the measured and observed volumes generated by the Oxylog 3000. Constant reassessment was required and ultimately successful in achieving adequate albeit not optimal ventilation Another issue was that we used the adult hosing system given the age of the patient, although the size of the patient may have indicated using the paediatric apparatus. I would be interested to hear others comments about this – the manuals suggests that paediatric circuits must be used in children but don’t suggest a weight cut off. I will contact a Drager representative to find out their recommendations (see discussion below).
[vimeo http://vimeo.com/37938870 w=640&h=385]
In conclusion, when using transport ventilators knowledge of your machine, adequate analgesia/sedation, constant reassessment and early expert advice can aid in achieving adequate ventilation in difficult cases.
Further Reading
(1) Slutskey A et al. Mechanical ventilation: lessons from the ARDS Net trial. Respir Res. 2000; 1(2): 73–77.
(2) The Acute Respiratory Distress Syndrome Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308
(3) Shirley P et al. Retrieval medicine: a review and guide for UK practitioners. Part 1: Clinical guidelines and evidence base. Emerg Med J. 2006 December; 23(12): 937–942
(4) Oxylog Manual (accessed April 2013) http://www.draeger.com/media/10/08/29/10082917/9066099_Oxylog_3000_plus_EN_170510.pdf
(5) Emergency Care Institute Introduction Video – http://www.ecinsw.com.au/oxylog_ventilators



Talk about permissive hypercapnea! I guess pH is more important that actual PCO2 here. Cutoff of 7.2 for safety but we’ve seen worst. They recommend bicarbonate for pH less than 7.2 though I disagree with that cocept cause it only translates to converting HCO3 to CO2 making things worse. I agree with maximizing ventilatory strategies to correct pH because at the end of it all it’s about ratios not about hCO3 and CO2 being treated individually. I was going to mention about recruitment trial(sustained inspiration) and prone position( try this during retrieval!!!)but based on the info given and blood gas I’m assuming this patient has more of an obstructive picture than an actual baby lungs though possibly a component of it. If I’m concerned of barotrauma, like what you did, I’ll intermittently press on that oxylog inspiratory hold button, keep RR down(gradually 10 then 8 possibly 6) keep I:E 1:4 if at all possible and keep the inspiratory time short. Also, keep FiO2 <70% (prevent O2 Tox). Again, let's treat the patient more than the numbers. I haven't done much pressure support with oxylogs. Do you guys have the same success with oxylogs in retrieval with PSV? Anyway, other non-ventilatory management strat are yet to be routine care, namely:Nitric oxide, steroids( though had one patient who had paraquat od tx with methylpred who did quite well), proper fluid management (bring out those ultrasound probes!) , HFOV subwoofers and ecmo! I'd
love to hear from Pressure support loving people.
Great topics Andrew. Keep it up.
Cheers,
Harry Elizaga
HI Andrew
Your blood gas machine suggests that your patient was particularly difficult to ventilate, but easy to oxygenate. I’d be interested to know more about the clinical context here – this looks like your acute severe asthma rather than someone with an oxygenation issue. You are ventilating him/her with 6ml/kg tidal volume per ARDSnet – but what PEEP are you using….? ARDSnet ventilation is more akin to the profoundly hypoxic patient and permissive hypercapnia is the rule. But here oxygenation isn’t an issue and you’ve got plenty of room to move. If you are retrieving, by all means sedate/paralyse, the use a mandatory ventilation mode with Pmax 35cmH2O, low PEEP (2-5cmH2O ish) and titrate FiO2 to pO2 that you’re happy with – but I think you should be able to increase your minute ventilation?
Secondly, I would not go treating a respiratory acidosis with NaHCO3 – it’ll just make things worse.
Cheers!
Alun
Hi Alun – I agree about the bicarbonate – although the acidosis was very severe, it seemed all ‘acute’ and ‘respiratory’ in origin – EMCRIT reviewed the use of Bicarbonate this week (1)
CLINICAL CONTEXT
In regards to the clinical context, the patient had no specific evidence of obstruction…
The CO2 trace looked normal to me – this chest had some mild creps at this bases but certainly no wheeze there…
The patient had CF but had a lung transplant 2 years ago.
I knew this at the time but I was really unclear as to the reasons behind this presentation and another similar presentation about 3 weeks prior.
Having discussed these issues with ICU doctors over coffee, the feeling is the patient might have had Bronchiolitis obliterans syndrome (BOS) (2)
The CXR was clear and as you said O2 was not an issue in this case…
It appears that most of the CF patients who get a transplant do quite well (3), but a significant minority develop BOS. A variety of management options for this have been suggested in refectory cases (4) (5) (6). Of course, in retrieval many of these options are not available or not directly relevant to the acute exacerbation of their disease.
VENTILATION
As I mentioned above prior to my arrival they were on a Puritan Bennet. Things were a struggle – the rate was 30 – on moving to the oxylog I started at 22 and eventually worked up to over 25 due to the worsening bloods gases – with a PMAX of 40ish and Plateau pressure of 28-32 we were able to hold the pH at about 7.1 and co2 in the 90s using the oxylog so we moved the patient but spent an hour in the referring centre practising “Oxylog Knobology”. All the usual optimising measures such as sedation and paralysis were used.
In the end we went to higher volumes (8-10ml /kg) in the patient – who weighed less than 30kg. The receiving team seemed happy with this given there was no evidence of barotrauma based on the Plateau pressure.
Regarding the circuit we used, having spoken with the company reps and our equipment officers it appears that the Paeds Circuits are used in those under 25kg. However, I have been advised that it doesn’t really matter too much except in Neonates. On this occasion we only had Adult Circuits available – I wonder if you thought this would make a difference?
In regards to PEEP this was set at 2, or 5 – I think it was 2 – and we checked and Expiratory Hold – no auto-peep
In conclusion, the take home points are that the Oxylog may struggle but is adequate for most patients with some tweaking, calling for advice is often helpful and transplant patients who are difficult to ventilate may have BOS.
Andrew
REFERENCE
(1) EMCRIT of HC03 Use – LINK: http://emcrit.org/podcasts/chloride-free-sodium
(2) Lung Transplant Complications Review http://ejcts.oxfordjournals.org/content/26/6/1180.long
(3) CF Lung Transplant – http://www.ncbi.nlm.nih.gov/pubmed/19010202
(4) HELIOX in BOS http://rc.rcjournal.com/content/58/4/e42.full
(5) OVERALL MANAGEMENT – http://journal.publications.chestnet.org/article.aspx?articleid=1088061
(6) MONTELUKAST – http://journal.publications.chestnet.org/article.aspx?articleid=1149042
Confirmed with the Drager reps that there are no major differences in what we discussed above with the OXYLOG 3000 and the new OXYLOG 3000 plus (the main additional features are the AUTOFLOW mode and the improved NIV functions)
I saw a vaguely similar scenario (though in a very different patient type recently) – Oxylog 3000 plus ‘pressure’ alarming and delivering insufficient tidal volumes in VC-SIMV.
Troubleshooting identified the culprit – Autoflow! Turning of the autoflow instantly normalised tidal volumes. The particular lung dynamics of this patient rendered this ‘feature’ a hazard, but it took us a little while to work this out – thankfully about 20 seconds before the ICU reg arrived…
Coming from an anesthesia-background and with such a ETCO2, Malignant hyperthermia caused by the RSI could also be something to consider.
Hi Andrew
I have just come off a night shift. Still tired of the 4.5 hours I spent between the oxylog and the BVM for a similar case.
This was a 65yrs old male with chr heavy smoking and 2 days of flu like illness (flu positive). His other BG has HTN, DM, cholesterol, ? Mitral prolapse but no COPD Dx. His weight was about 80kg.
After watching him tiring and building a co2 of 70 despite BiPAP, I intubated him and bagged him with absolute ease.
The troubles started when we moved to the oxylog 3000.
His ETCO2 got stuck between 90-130. His other vitals were within normal.
The consensus oxylog settings were SIMV/CMV, PEEP 10, VT 500-600, RR 18-20, I:E 1:3 on FIO2 40-60%. His VTe was always between 230-250 no matter what we did.
Also, the minute volume would suddenly sink from 8 to 1.5 and would then recover to about 4 within 5min or so.
His ABGs kept showing a significant respiratory acidosis. His CXR had cardiomegally but no major lung infiltrate.
We changed to another oxylog 3000, same story, and then oxylog 3000 plus and same happened.
And once we were ETCO2 of 120-130, frequent ectopics started to appear.
There was no ICU SR onsite and the advices that I got over the phone were all in line with the above.
So I basically needed, at the end, to take him off the oxylog completely and just bag him for the rest of the night, support his BP with a bit of fluids and metaraminol, while juggling through the full ICU, other hospitals ICUs and the retrieval service that doesn’t cover me between 12 and 8am. And .. this was a handed over patient.
Bagging him brought his ETCO2 to 60-80 on the expense of dropping the BP.
Once in the ICU, their totally different and big ventilator had absolutely no issues with ventilating this man using the exact same settings mentioned above and the same ETT.
Patient had also had fentanyl+midaz & vec, steroids, Mg, & salbutamol infusion. Patient’s tubes, connections, etc were all checked and confirmed in the ED.
Mild to moderate air trapping was clinically apparent in this case. ETT was repeatedly checked for leaks and none was found.
I am still doing my research about this and thought of sharing it here. Happy to read any comments or links you guys consider helpful.
Thank you
Arsalan