
We present 6 practice x-ray cases from Junior Medical Officer teaching at Westmead hospital. When interpreting films pattern recognition is developed quickly over time but always stick with your solid system so as to not miss things. FOAMed images from LITFL.
Lecture Handout Notes – CLICK HERE
Thanks for Dr Andrew Baker for the opportunity to present.

Case 1
- You are called by the nurse on the ward to check position of NG tube
- Where is the Nasogastric Tube?
- Where should it be?

Answer – Look for the “tip” 10cm below the Lower Oesophageal Sphincter:

Are you happy to feed the patient without repositioning?

No. Not in this case!
This patient developed an aspiration pneumonitis after enteral feeding into the lung…

Case 2
- A normally healthy 33 year old man is brought to your Emergency Department with acute shortness of breath after developing chest pain during a run at the park.
- On arrival in hospital, he is pale and sweaty. He was found to be tachycardic and hypotensive. A CXR was taken immediately after a procedure was performed to stabilise his condition.

Can you describe his Chest X-ray?
- Chest X-ray showing a pneumothorax
- A thoracotomy needle in the left chest
- No evidence tension pneumothorax (deviated heart, mediastinum, trachea)
Can you write down a systematic approach to interpreting a Chest X-ray?
- Demographics (Name, Time Taken)
- ‘Rotation’
- –(Quality = Rotation/Adequacy/Penetration)
- Apparatus
- Airway (Trachea)
- Breathing
- Mediastinum (>7cm)
- Hilum (Left Should be Higher than Right)
- Lungs (Lung Fields, Fissures)
- Circulation
- Diaphragm
- Everything Else
- Step Back – Consider ‘Overall Appearance’ (‘gestalt’ comes in here)
What are your treatment options?
Resuscitation Phase

(1) Is there is evidence of tension pneumothorax?
- IV, O2, Monitor
- Decompress the pneunothorax with needle +/- aspiration technique
- Follow the A-G assessment
- Call for help

General Manangement
(2) Are there minimal symptoms?
- YES
- If small (3cm or less at hilum) – observe (oxygen may increase absorption)
- NO – patient is symptomatic
- follow BTS guideline
- consider a chest drain if >3cm
(3) The patient is not improving after chest drain for several days – what should I do?
- Get a CT scan to reveal a possible underlying cause for the pneumothorax
- Involve a Cardiothoracic surgeon in the care (may need surgical intervention)
Approaches to Pneumothorax for reference:


Case 3
- A 60 year old car driver presents following a head on collision with a bus at 60Kph.
- Her observations are listed:
- HR 98
- BP 130/90mmHg
- Respiratory Rate 24/min
- Oxygen Saturations 98% (on 6L oxygen)
- Afebrile

Describe and interpret her X-ray
- Widened Mediastinum
- Clavicle Fracture
- Rib Fractures
- ?Right Haemopneumothorax
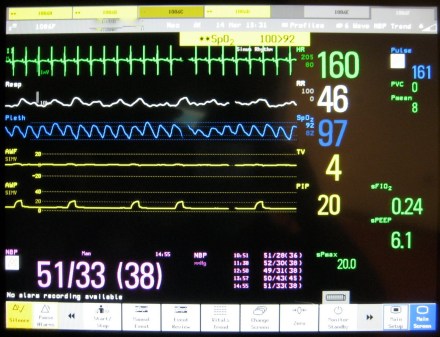
Outline your management options
- Care of the Trauma patient is delivered by a Team with good communication amount members. Ultrasound would help you differentiate the chest injuries further in skilled hands
- Start treating the patient with the mantra IV / O2 / Monitor with resuscitation trolley at the bedside
- Restore the patient’s blood volume
- If shocked (as the picture above would indicate) activate your local transfusion protocols in liaison with haematology
- If Aortic Injury is a concern caution with over resuscitation
- Chest drain (intercostal catheter insertion) of the correct side – re-expansion of the lung may help tamponade bleeding
If Aortic Injury:

- Thoracotomy for haemothorax – if on going bleeding or massive initial blood loss
- Disposition – admission to ICU

Case 4
- A 65 year old woman presents to your hospital with gradually increasing breathlessness over the preceding 2 days.
- It is about 10 days since her last chemotherapy (cisplatin).
- Her observations are:
- BP 130/70,
- Respiratory rate 30/min
- Oxygen Saturations 91% (on 6L Oxygen)
- Temperature 36.8 degrees
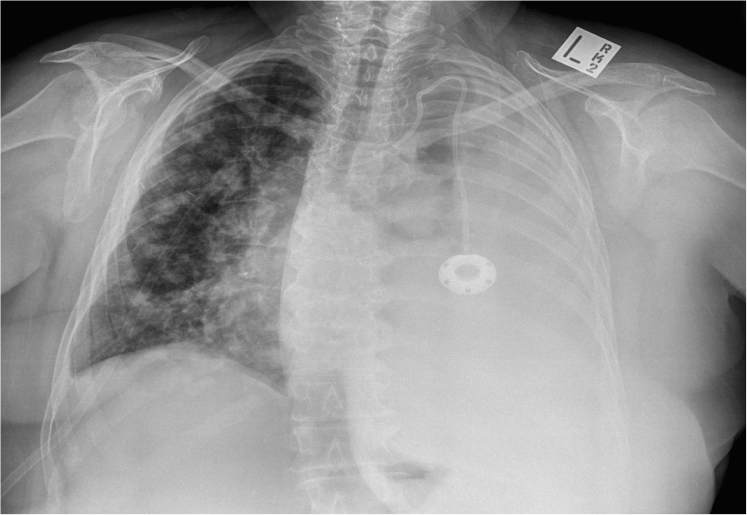
What does her Chest X-ray show?
- Large left pleural effusion
- Multiple discrete lung parenchymal lesions typical of metastatic lung disease
- Portacath
- ? Mastectomy
- ? O2 Mask
- No Obvious boney mets
Write down 6 differentials in the acutely short of breath patient with malignancy
- Sepsis with metabolic acidosis (in view of recent chemotherapy)
- PE
- Pericardial Effuson
- Pneumonia
- SVC Obstruction
- Pleural Effusion(s)
- Lymphangitis
What are the causes of a Pleural Effusion?
- Transudates – Congestive Heart Failure, Liver Failure, Renal Failure, Nephrotic syndrome, Hypoalbuminaemia, Enteropathy and Dialysis
- Exudates – Lung Ca, TB, Infections (Bacterial), RA, Pancreatitis, Sub-phrenic Abscess, ‘Meig’s’ Syndrome, Dressler’s Syndrome, SLE, Lymphoma, Hypothyroid, PE, Mesothelioma, Yellow Nail Syndrome and Vasculitis
What is Light’s Criteria?
- According to Light’s criteria a pleural effusion is exudative if at least one of the following exists:
- The ratio of pleural fluid protein to serum protein is greater than 0.5
- The ratio of pleural fluid LDH and serum LDH is greater than 0.6
- Pleural fluid LDH is greater than 0.6 times the normal upper limit for serum. (i.e 0.6 of 200)

Case 5
A 50 year old regular Emergency Department presenter with a history ETOH excess presents with a few weeks of feeling tired and coughing up small amounts of blood. He has a past history of pancreatitis and appendicectomy

What does the X-ray show?
Answer – X-ray showing a ‘cavitating’ lesion in right chest with soft tissue densities in lower zone.
List your differential diagnosis
- Some of the causes include:
- Acute Infective causes – such as TB, Fungi, Aspiration
- Malignancy (Primary and Secondary)
- Abscess
- Other bacterial infections Staphylococcus / Klebsiella
- Wegner’s (recent name change of this disease due to a Nazi doctor who described it)
- Severe Fibrosis
- PE

Case 6
- PICC lines are occasionally required for venous access IV administration of medication nutrition.
- You are called to the ward for a patient who has just had a PICC line placed.
CXR (http://www.rtexam.com) is shown:
Are you happy with the position of the PICC line?
- Chest X-ray showing tip of PICC line in the Superior Vena Cava (SVC) – so in this case we are happy with the position
- Malposition of the tip is common (superior (IJ), across (subclavian), or twisted around). In one study about 8% of PICC lines were badly positioned on initial assessment post insertion
- Feeding / medications should not be commenced unless a good position is identified on the CXR

References
(1) Image 1 – Click Here
(2) Image 2 – Click Here
(3) Image 3 – Click Here
(4) Image 4 – Click Here
(5) Image 5 – Click Here
(6) Image 6 – Click Here

Great post! I recommend attributing/citing sources from which figures are obtained. This serves several purposes and allows readers to contact primary authors should a change or typo exist. Thanks for the #FOAMed.
Thanks . If you click on each item it should take you there but we ll add a fuller reference section at end. This was really an intern flipped classroom more than anything else…