Part I – Aortic Dissection (AD)
A 68 year old woman is brought to your emergency department (ED) from a shopping centre where she had sudden onset chest pain and a syncopal episode.
On examination there is no evidence of trauma.
- Observations:
Blood Pressure 97/40, Respiratory Rate 20/min
Heart Rate 125, Temperature 37.1 degrees, Oxygen Saturations 97%
(on 8 litres by Hudson Mask)
Write down four critical diagnoses you would consider and one risk factor that is associated with each of these diagnoses…
MI, PE and Pneumothorax come to mind but would you consider Aortic Dissection as a cause in this patient?
The 12 lead ECG shows sinus tachycardia
Here is the patient’s Echocardiogram and CXR:
CXR shows a widened mediastinum and the echo shows a proximal dissection flap
CT angiogram confirms the diagnosis of a “Stanford A” aortic dissection.
How would you treat this patient in the ED?
Key Issues
- High Index of Suspicion is required for Diagnosis
- Determine the anatomy of the dissection (e.g. Stanford A or B)
- Move to Resuscitation Bay
- IV, O2, monitor, ALS equipment to hand
- BP control
- Beta Blocker and Vasodilator (need to reduce HR and wall stress)
- Urgent Surgical Referral
- Early referral to a cardiothoracic centre if in rural area or smaller hospital
- Emergency Surgery Preparation in the ED (NBM)
- Analgesia (e.g. Titrated Fentanyl IV)
- Cautious Resuscitation with fluids (as required)
- Good Supportive Care
- Place lines and get consults from ICU and anaesthetics
- Avoid Anticoagulation (doubles mortality)
- Handout on Aortic Dissection – Aortic Dissection

Part II – Aortic Traumatic Injuries
PDF Handout – AORTIC INJURIES
Introduction
Injury to the thoracic aorta is an important cause of death and disability following significant blunt trauma.
Three main types of injuries can occur (see figure below).
Possible injuries include complete transection (invariably leading to death), aortic haemorrhage as well as more occult contained injuries. Aortic Injury is relatively common but many patients will die prior to arrival in the Emergency Department. Some patients may present latently (or not at all) if the diagnosis is not considered in the initial evaluation of the trauma patient.
“Contained aortic injuries may be ‘stable’ at arrival in hospital so require a high index of suspicion to diagnose”
Aortic tears are often associated with other traumatic injuries. The cause is usually a rapid deceleration due to high energy traumatic forces such as a Motor Vehicle Accident (MVA). Severe trauma creates a shearing force which can tear the Aorta. Relatively low impact injuries can also cause traumatic Aortic Injury especially in older patients.
Anatomy
While any portion of the aorta can be injured the proximal thoracic aorta is the most common location. More specifically, the proximal descending aorta is often injured. In the proximal descending aorta the relatively mobile aortic arch can move against the fixed descending aorta.

Mechanism of Injury
The transitional portion of the Aortic Arch is at greatest risk from the shearing forces of sudden deceleration. This part of the Aortic Arch is known as the ligamentum arteriousm. Classically, Aortic Injury is more common in falls from a great height and high energy MVAs with heavy impacts or rollover. Traumatic Aortic injury has also been postulated to be due to compression (osseous pinch) of the chest or sudden arterial pressure change.
Medical Imaging
Chest X-rays (CXR) have been traditionally been used to evaluate major chest trauma. A massive left haemothorax may indicate the presence of a significant Aortic Injury.
The following CXR demonstrates severe left chest trauma – Aortic Injury should be a concern in these circumstances:
An entirely normal chest x-ray is somewhat reassuring in the first instance but unfortunately many CXRs in the Emergency Department are either inadequate or have non-specific abnormalities. So while CXR is a very useful test in chest trauma it may miss up to 11% of patients with Aortic Injury if used alone as a single test to exclude this injury. When you look retrospectively at patients with a proven Aortic Injury up to 50% have no specific findings on their CXR.
Definitive rule out of Aortic Injury requires Helical Computerised Tomography (CT) scanning with appropriate contrast. Patient selection for CT is often based on mechanism of injury and is generally indicated in “high risk” patients with a concerning mechanism of injury. In addition, patients with associated injuries on their initial assessment should undergo CT scanning to exclude Aortic Injury. A normal CT essentially rules our traumatic Aortic Injury. Signs of injury on the CT scan include direct (e.g. aortic disruption, visualised flap and false lumens) and indirect (e.g. mediastinal hematoma and abnormal aortic contour).
Historically, the downside of CT aortograms is their lack of specificity (83%) and relatively low positive predictive value (65%). With new generation CT scanners this may be less of an issue but where doubt remains we should consider a formal aortogram and/or echocardiography to confirm the diagnosis.
Associated Injuries
Since the 1970s 1st Rib Fracture has been seen as a hallmark of severe trauma. According to Gupta (1997), when seen in the context of major trauma there was vascular injury in 24% of patients with 1st Rib fracture. In the same study it was noted that isolated 1st rib fractures were relatively benign.
Sternal and Thoracic Spine fractures are often associated with severe blunt trauma and their presence should also raise suspicion of a significant underlying occult injury such as an Aortic Injury.
Scapula Fractures have also been associated with significant underlying chest injury including Traumatic Aortic Rupture.
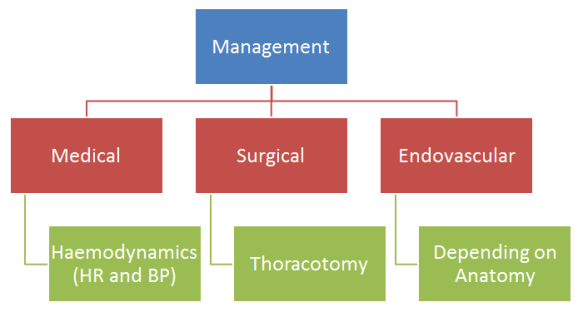
Management
- General Management:
- Early Recognition
- Consider Aortic Rupture in the patient that transiently responds to fluid resuscitation and has an abnormal CXR and/or a left haemothorax
- Optimise ventilation
- Single Lung ventilation may be required during surgery
- Haemodynamic Monitoring
- Usually using an arterial line and continuous ECG monitoring
- Blood Pressure Management
- Control both the luminal pressure (BP) and number of beats (heart rate)
- Conservative Management may be indicated in some cases and management is often delayed due to other injuries such as head and abdominal trauma.
- Early Chest Tube where appropriate (see below)
- Early Recognition

- Surgical Management:
- Intercostal Catheter (ICC)
- Measure the ICC output carefully
- Close Observation in a High Dependency setting
- NB – Smaller Tubes may be okay (Inaba et al)
- NB – Not all chest injuries need an ICC
- Thoracotomy
- Required in the patient who is haemodynamically unstable (from the Aortic Injury)
- Challenge with this rare operation is skills maintenance for the Trauma Surgeons
- High complication rates
- In one study 211 patients underwent open surgical repair with a high morality (31%) observed and high rates of neurological deficit following the Thoracotomy. (Post-op paraplegia was observed in 8.7%).
- Intercostal Catheter (ICC)
- Endovascular Management:
- Endovascular repair is now a standard approach to repair of many Aortic Injuries.
- Specific anatomical caveats apply to the use of an endovascular repair.
- It is generally faster and associated with less complications compared to open surgical techniques.
- Stents are designed for aneurysm repair and we don’t have good data on long-term outcomes in younger patients.
More Resources on Traumatic Aortic Injury
Prof Colin Graham (Hong Kong)
EAST Guideline (USA)
Trauma.org (UK)
Management Overview (USA)
Crashing Patient (USA)




One thought on “Aortic Injuries and Aortic Dissection”
Comments are closed.