Emergency Medicine
Soft Tissue Infections
Overview
While rare, Necrotising Fasciitis and Soft Tissue Infection associated with Septic Shock are important considerations in the Emergency Department (ED).
Necrotising Fasciitis carries a high mortality (over 25%) especially when definitive treatment is delayed. Therefore, when suspected early “medical” and “surgical” treatment are both very important.
Recognition of the disease requires the physician to consider a diagnosis of Necrotising Fasciitis in any patient with cellulitis in the ED. A high degree of concern should be focused on patients with severe pain, severe swelling or severe skin changes and/or signs of systemic inflammatory response (SIRS).
While rapidly progressive soft tissue infection can affect any part of the body it is important to look particularly at the upper and lower limbs, perineum (Fournier’s gangrene) and abdomen (very high mortality).
Which patients are at risk of developing time critical soft tissue and skin infections?
-
Classically Diabetic Patients are at increased risk
-
Excess Alcohol Consumption
-
Intravenous (IV) Drug Use
-
Immunosuppression (medications or underlying pathology)
-
Chronic medical diseases (e.g. liver failure and renal failure)
-
Recent Surgery
-
Methicillin Resistant Staphylococcus Aureus (MRSA)
-
Obesity
Necrotising Fasciitis – Click Here
Fournier’s Gangrene (2006 FACEM VAQ Exam) – Click Here
Surgical Cellulitis (other VAQ) – Click Here
What is Sepsis and why is it important?
Sepsis accounts for a huge number of deaths worldwide and accounts for a large number of admissions to hospital in Australia. In severe cases patient are admitted to the Intensive Care Unit (ICU) and despite recent improvements in recognition and early treatment sepsis remains a serious clinical problem with a high mortality.
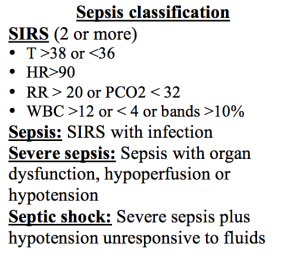
Infective pathogens can cause of deleterious inflammatory response. This is due to a “cascade” and proliferation of inflammatory mediators such as cytokines. Systemic Inflammatory Syndrome (SIRS) describes a combination of clinical parameters associated with potentially harmful consequences. SIRS is overly sensitive and does not predict severe or life-threatenintg sepsis (and has been criticised) but does provide a useful common language for early recognition in the ED.
Sepsis is simply defined as SIRS PLUS evidence of an Infectious Process (such as soft tissue infection):
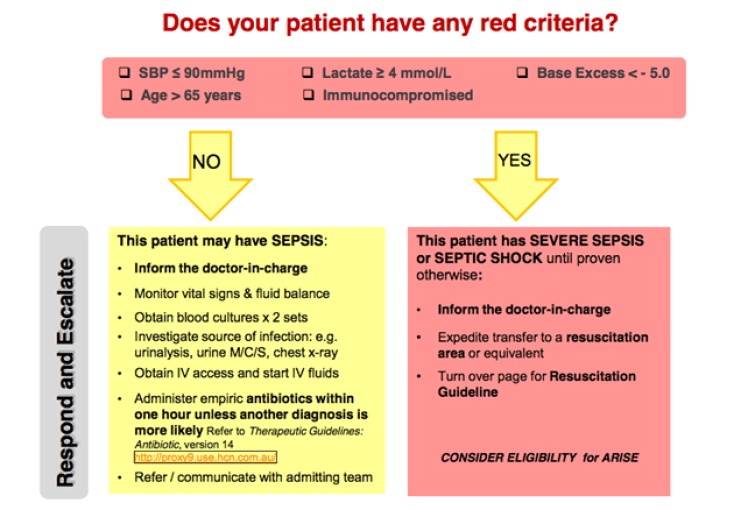
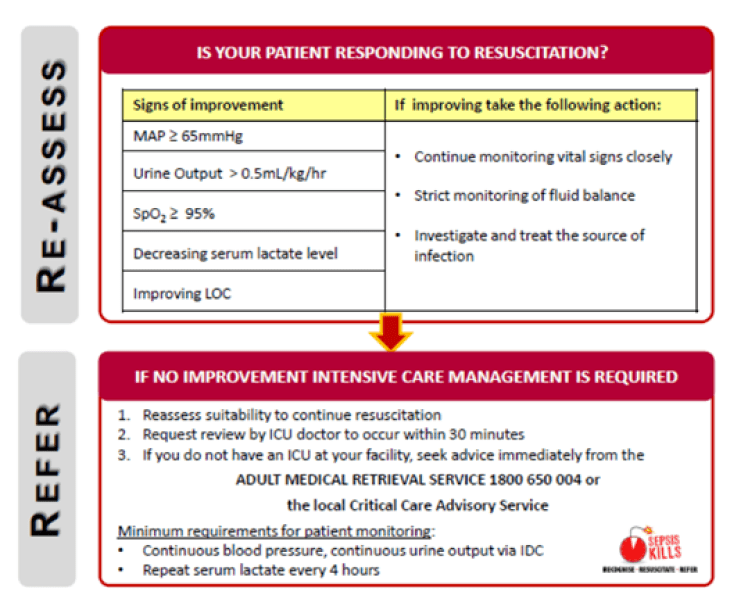
Severe cases of Sepsis are associated with Multi-organ Failure and protracted ICU admission. Severe Sepsis is associated with short and long term mortality. Predicting Severe Sepsis in the ED is challenging but use of early Lactate and Blood Gases along with Clinical Prediction Scores can be useful. Education in the importance of sepsis and good clinical governance are also very important. The following Sepsis Pathway has been rolled out in Australian Emergency Departments as part of the “Sepsis Kills” campaign and will expand to ‘the whole hospital’ in 2014.
Recognition of Sepsis (**)
Respond to Suspected Sepsis
Re-assessment and Referral of the Septic Patient
**Updated Sepsis Pathway (2016) – CLICK HERE
What are the symptoms and signs of Necrotising Fasciitis?
- Severe symptoms associated with any soft tissue infection should raise the suspicion of Necrotising Fasciitis (“an Emergency Surgical Cellulitis”).
- Some patients may have a delirium or indifferent affect associated with highly abnormal appearances of areas of soft tissue infection.
- Signs include the following
- Tachycardia and Hypotension (common)
- Lack of Sensation to the affected area
- Malodourous Smell(s)
- Extensive Skin changes (e.g. Discharge, Oedema and/or Blistering)
What investigations help make the diagnosis?
Key Point – Diagnosis is based on CLINICAL grounds.
Investigations may aid in the diagnosis and/or raised the index of suspicion:
- Bedside
- BSL (High – Diabetic at risk patient), ECG (tachycardia) and Urine
- Imaging
- X-rays showing gas in soft tissues. Ultrasound (collections).
- Laboratory Tests
- High White Cell Count (WCC) with Neutrophillia (almost universally found)
- High CK
- High Lactate and High Anion Gap Metabolic Acidosis (get an early blood gas)
- Inflammatory markers such as CRP and PCT.
- Look at LFTs and EUC (i.e. is there Multi-organ Failure?)
- Later Tests
- CT Scanning and/or MRI of Extremities
What is the management of suspected Necrotising Fasciitis in the Emergency Department?
Overview
A time dependent surgical emergency with a high mortality requiring multidisciplinary input.
ED Priorities
Early Recognition
Early Referral for definitive care (e.g. a Surgical debridement)
Resuscitation Care
- Attach Monitoring to the patient
- Patient likely to be Critically Unwell
- Assign Key Team Roles to the treating medical and nursing team staff
- Treat in Resuscitation Area/Cubicle/Bay
- Titrate Oxygen Therapy
- Adequate Intravenous Access
- Send the lab 2 sets of blood cultures and prioritise antibiotics
- Initiation of a Sepsis Pathway (discussed above)
Specific Care
- IV antibiotics – Broad Spectrum (covering Gram +ve, Anaerobic, Gram –ve and MRSA)
- e.g. Extended Spectrum Penicillin (Tazocin) or Carbapenem (Meropenem)
- plus Glycopeptide (Vancomycin)
- plus Aminoglycoside (Gentamycin)
- IV Fluids
- Crystalloid (e.g. Hartmann’s or Normal Saline)
- 20-30ml/kg Bolus – titrate to Urine Output, Lactate and Mean Arterial Pressure (MAP)
- IVC Ultrasound and other methods for Prediction of Fluid Responsiveness
- Judicious Analgesia
- e.g. Fentanyl 1mcg/kg slow pushed bolus titrated
- Definitive Surgical Drainage
- call surgeons immediately, emergency wound exploration may aid in confirmation diagnosis
- Intravenous Immunoglobulin (IVIG)
- may have a role in severe cases (liaise with ICU)
- Inotropes
- patients are often hypotensive and have Multi-organ Failure (MOF)
- Invasive Monitoring
- Arterial Line (measure MAP – aim >65mmHg and look of variance in the blood pressure)
- Central Line (monitory central venous Oxygen Saturations – maintain>70%, limited use of CVP)
Supportive Care
F – Fluids (discussed above, consider albumin after ‘adequate’ fluid resuscitation with crystalloid)
A – Analgesia (discussed above – should be multimodal)
S – Sedation (if intubated provide adequate analgesia and sedation, avoid exacerbating delirium with oral medication)
T – Thromboembolic Prophylaxis (as hospital protocol)
H – Head of Bed (position patient comfortably in bed)
U – Ulcers (e.g. avoid pressure points on back and provide a PPI for peptic ulcer prophylaxis)
G – Glucose (e.g. monitor BSL carefully, consider Insulin infusion)
I – In-dwelling catheter (IDC) – monitory urine output and aim >0.5ml/kg/hour
N – Nasogastric Tube (NGT) – if intubated
B – Bowels (e.g. examine abdomen and look for ileus)
E – Environment (e.g. well lit room, good nursing care, good communication with patient and family)
D – De-escalation of care as appropriate (e.g. advanced directives)
Please – Provide adequate Psychosocial Support
Disposition and Consultation
- Key Consultations
- Emergency Department Seniors, Surgical Team, Infectious Diseases Team, Intensive Care Unit Team
- Disposition
- Intensive Care Unit after Debridement in Theatre
Conclusions
In conclusion, detecting severe and life-threatening soft tissue infections in the Emergency Department requires a high index of suspicion in ‘at risk’ patients.
Successful management in the ED includes early antibiotics (medical) and debridement in theatre (surgical). All treatment should be initiated early in the patients presentation because of the high mortality and therefore recognition is crucial.
References and Further Reading
- ED Surgical Emergencies Review Article – Click Here
- EMRAP TV – Video Overview of Severe Soft Tissue Infections – Click Here
- Revised Surviving Sepsis Campaign Guidelines (2012) – Click Here
- 2006 FACEM VAQ 1 – Click Here
- 2006 FACEM VAQ 2 – Click Here
- Clinical Excellence Commission (CEC) Sepsis Australia – Click Here
- SIRS Criticism
- 1) Click Here
- 2) Click Here
- Albumin in Sepsis – Click Here
- Arterial Blood Pressure and Variation – Click Here
- Fluid Responsiveness – Click Here
- CVP Review – Click Here
- Arterial Blood Pressure – Microcirculation versus Macrocirculation – Click Here






Hello sir,
Thank you for your nice posting.detecting severe and life-threatening soft tissue infections in the Emergency Department requires a high index of suspicion in ‘at risk’ patients.
Thanks….
New version of the Sepsis Pathway has been out for a while – http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0004/259411/sepsis-newsletter-winter-2014.pdf
Sepsis 3.0 with Dr Singer – http://emcrit.org/podcasts/sepsis-3