HUMAN FACTORS
Human Factors in Critical Care
In the ED chaos is common. In the management of many emergencies the default situation can be chaos unless a concerted effort is made to gain control. A loss of control in a crisis can in turn can lead to dilution in the quality care of our sickest patients and therefore we need training in dealing with crises… Working in a busy Emergency Department and doing a retrieval medicine has taught me that models of care and checklists are complementary to providing good critical care. This is especially true in variable environments with a variety of team members working together often for the first time and in stressful conditions.
HUMAN FACTORS REVIEW

Prior to any Medical Emergency assemble a Team as early as possible – complete a P.A.E.D.S. Checklist:

Critical Care is not limited to the ICU.
But the location can be a challenge…
Basic critical care concepts can be confusing and difficult to apply outside of the Intensive Care Unit (ICU) setting. Exposure to Emergency Medicine and pre-hospital environments help in understanding the process of applying critical care concepts in the non-ICU setting. For example placing a central line at 10am after a ward round in ICU in controlled manner is different to placing a central line (with USS to a high-standard of sterility) in the ED prior to moving a critically unwell patient to theatre for urgent surgery. Time pressure, other resuscitation activities and immediate necessity all contribute to difficulties in this example.
To maintain control it is important to consider 3 factors (in advance of managing an Emergency situation):


PRE-HOSPITAL & RETRIEVAL MEDICINE (PHARM)
The Pre-hospital and Critical Care Interface
Here are 4 lessons I am using and will take away from my time in retrieval medicine:
AIRWAY MANAGEMENT CHECKLIST
The use of a Rapid Sequence Intubation (RSI) checklist helps in the sharing of the clinicians thought processes, efficiency of teamwork and preparedness for managing a difficult airway. We use the RSI Checklist from the Excellent GSA HEMS RSI Handbook: CLICK HERE
I plan to continue a checklist for all intubations in the Emergency Department (ED) with the exception of patients in Cardiac Arrest and also plan to recommend this to my ED colleagues too.
Similar models and intubation checklists have been adapted to the ED setting by Dr Toby Fogg at Royal North Shore Hospital: CLICK HERE

BREATHING
- Many of us have heard that a lung protective strategy is the standard care for patients post-intubation in the ED
- This is based on the ARDSnet data and meta-analysis of controlled trials on various ventilation strategies
- How do we best achieve this in the busy ED using our equipment?
It’s easy to forget basics like Patient Positioning (30 degrees) and Adequate Analgesia/Sedation. Analgesia is a good place to start.Involving the ICU doctors at an early stage can be helpfulI also found the Drager Online Program useful – CLICK HERE
- Knowing your equipment is essential to success:
- Intubation Equipment
- Ventilators
- Defibrillators
- Cannulation Equipment, Central Lines, Arterial Lines and Intraosseus Needles
Ventilators
Further Reading – CLICK HERE
youtube=http://www.youtube.com/watch?v=AVev0DYYWQ4
CIRCULATION
During time working in retrieval medicine several concepts were emphasised and now feel more familiar especially the use of Inotropes in the Pre-hospital and Inter-hospital setting:
- Experience Appropriate use of Inotropes included the following:
Noradrenaline is the Inotrope of choice in Septic Shock and SIRS – CLICK HERE
Use of Adrenaline Infusion may be required in Neurogenic Shock – CLICK HERE
In general not using Metaraminol or other Ionotropes in Trauma patients (use blood)
Double Pumping (see 5mins into the the video embedded below discussing patient transfers)
Inter-hospital Patient Packaging
This is also very relevant to moving patients around the hospital (to CT and between departments):
POST INTUBATION AND SUPPORTIVE CARE
Supportive Care
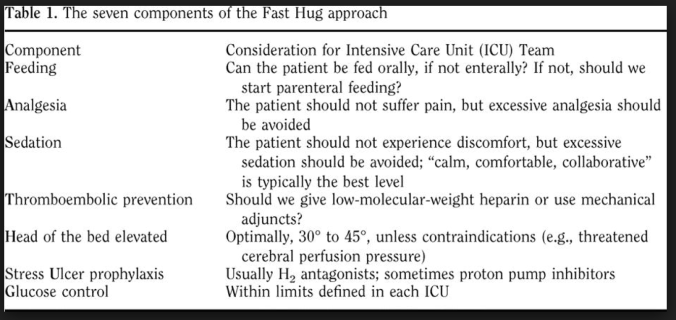
“F.A.S.T.H.U.G.” is a commonly used approach to supportive care in the ICU ensuring that basic patient management needs are met on a daily basis. We suggest that you give critically unwell patients a “FASTHUG IN Their BED” both in and out of the ICU.
Additions to ‘F.A.S.T.H.U.G.’ for the Emergency Department
- Skin and Wound Care, Suctioning
- IDC and Continence Care
- NGT or OGT
- Touchy Feely Fluffy Bunny Stuff (Psychosocial Support)
- Bowel Movements
- Environment
- Deescalation of Care
The original FASTHUG approach:





Particularly like the Oxylog chart Andrew.
Everyone ventilated on a volume mode should be getting 6ml/kg IBW tidal volumes with decent PEEP (if they can tolerate) even if they don’t have ARDS – although as the chart points out this does not apply to those with airflow limitation and dynamic hyperinflation, as seen in acute severe asthma and some COPDers.
Ref: Determann et al, Crit Care 2010 14:R1 (note this was published before the Berlin criteria, which is slowly being adopted down under)
Hi Alun, thanks for your comment.
I agree that a routine lung protective strategy is the way to go with all patients except those with severe asthma and COPD.
The Asthma patients, in my limited experience, are at high risk – and near on impossible to ventilate with the Oxylog 3000 (even with the improvements such as auto flow on the 3000 plus I doubt this machine would be different). It seems to perform well in most other patients though.
In the retrieval setting (inspiration for this post) I have found mixed knowlege around the state when it comes to post-intubation management. Typically, patients are getting in the range of 6-10ml per kilogram. It would be interesting to do a survey (like your Sedation and Analgesia survey: http://expensivecare.com/2013/01/20/is-propofol-really-that-bad).
Let me know your thoughts.
Andrew
VAF mode on the Oxylog is very useful in minimising exposure to high ventilatory pressures. Ventilation of the asthmatic is a science unto itself as they exhibit very different lung behaviours to your standard ICU patient, but I expect most retrieval clinicians are not familiar with it and are likely to ventilate on a PCV mode with the patient heavily sedated and with neuromuscular blockade, on an I:E ratio of 1:4 or something. Low or no PEEP in this case. I would prob sedate with Midas/ketamine plus rocuronium or cisatracurium infusion (being less histaminergic), plus all the other unproven drugs being infused. Oxygenation is never really a problem… The most useful thing on route would be to watch gas flow patterns on the ventilator for gas trapping – ETCO2 is unreliable. Interested to hear your thoughts Andrew!
VAF probably isn’t the ideal go-to mode however for acute severe asthma as the volumes you prescribe may not be achievable with such poor lung compliance and there is a risk of hyperinflation. Should have pointed that out! Not great either in severe ARDS (for similar reasons) but I think it’s very useful most other lung disorders.
Agree with everything you said! I would be calling you for help in Acute Severe Asthma ventilation! I’d certainly have them on a Salbutamol +/- Adrenaline Infusion at this stage. I am usually watching there BP closely (arterial line) as well at the ETCO2 waveform shape. Do you think there’s a role for Heliox?
Hi Andrew – missed this one. Not sure I’d see the rationale with a selective B2 agonist and a non-selective A/B agonist unless you’d want circulatory support. I’d keep it simple and choose one or the other.
ETCO2 is pretty useless in acute severe asthma. All it tells you is that the tube is in and the heart is pumping. The airflow limitation would make interpretation difficult. The pressure/volume/flow curves on your Draeger are more clinically useful and I think you’d do more harm than good trying to chase a particular CO2.
Haven’t ever seen/used Heliox, think the evidence is pretty patchy. You’d need a Heliox ratio adequate for oxygenation of course if you were planning on using it.